I. INTRODUCTION
Somatic symptom disorder is a disease in which mental conflict is expressed as somatic symptom. In the DSM-5, a somatic symptom disorder has one or more somatic symptoms that are distressing or result in significant disruption of daily life. Also, one or more of disproportionate and persistent thoughts about the seriousness of one’s symptoms, persistently high level of anxiety about health or symptoms, and excessive time and energy devoted to these symptoms or health concerns appear. It is characterized in that the state with these symptoms persist for more than 6 months1).
Patients with somatic symptom disorder can complain of various somatic symptoms across all organs, and it is difficult to find an organic cause for the symptoms. Symptoms can be inconsistent, dramatically exaggerated, and expressed in a variety of ways2). Anxiety and concern about somatic symptoms can be overwhelming. In addition, depression or anxiety disorders can be associated with somatic symptom disorders1,3).
Somatic symptom disorder is a disorder first defined in DSM-5, and encompasses all of DSM-IV-TR’s somatization disorder, undifferentiated somatoform disorder, pain disorder, and hypochondriac symptoms accompanied by somatic symptoms of hypochondriasis. Among these disorders, the basis of somatic symptom disorder is somatization disorder. Somatic symptom disorder in DSM-5 differs from somatization disorder in DSM-IV-TR in that it does not require age, number of somatic symptoms, and symptoms that are not medically explained, and focuses attention on stress caused by somatic symptoms and the resulting non-adaptive disease behavior3).
In Korean medicine, there are no symptoms that clearly correspond to somatic symptom disorders, but when considering the pathogenesis factors and diversity of symptoms, several corresponding symptoms can be considered. When humans are under stress, mental and somatic reactions appear. According to epistemology of ‘body and mind as one (心身一如)’ in Korean medicine, stress phenomena such as seven kinds of pathogenic qi (七氣), nine kinds of pathogenic qi (九氣), qi depression (氣鬱), and qi counterflow (氣逆) occur due to changes in seven emotions (七情), a specific phenomenon of mental function, and it is considered that pathological symptoms occur by acting on various body organs4).
Meanwhile, as the number of traffic accident patients and medical expenses continue to increase due to the recent increase in the use of automobiles in Korea, the scale of medical treatment at Korean medical institutions is also increasing5). In addition to surgical pain, many traffic accident patients complain of systemic symptoms such as systemic weakness, dizziness, and neuropsychiatric pain such as anxiety and depressive disorder6). Therefore, neuropsychiatric approach is necessary for traffic accident patients in Korean medical institutions.
In Korea, there are various case reports published by Seo7), Kim8), and others about somatic symptom disorder or somatization disorder. However, no cases of Korean medical treatment have been reported for patient whose symptoms of a somatic symptom disorder were worsened after traffic accident.
We report that patient with somatic symptom disorders worsened after traffic accident received improved results by performing Korean medical treatment during hospitalization.
This study was granted review exemption in accordance with the review exemption criteria of the Institutional Review Board of Dongguk University Oriental Hospital (DUBOH 2020-0008).
II. CASE
2. Chief complaints
Both upper extremities pain, both lower extremities pain, headache, nausea, chest discomfort.
4. Mode of onset
She was driving in the rain at the time of the traffic accident, and the car coming from the other side slipped. The right side of the opponent’s car and the front part of the patient’s car collided, causing an accident. At that time, the seat belt was worn, and after the accident, she injured her forearm, both knees, and both upper arms in an accident.
5. Present illness
Even before the accident, she intermittently complained of throat discomfort (a feeling of lump around the throat), a tingling and pulling feeling around her left face, chest discomfort (feeling blocked up in the chest and palpitation), and tension of whole b ody. She s aid that she i s sensitive to a stress, and that when she is stressed, the somatic symptoms well worsen. She had problems with her daily life because of these somatic symptoms. She did not complain of somatic symptoms just before the accident, but said that the somatic symptoms became very severe after the accident.
After the accident, she was taken to the emergency room of a university hospital and was taken CT (Brain, Facial, Chest, Abdomen, Pelvis, C-spine, Knee, Elbow, Wrist), X-ray (Chest, Pelvis, Knee, Elbow, Wrist, Hand), and MRI (Knee). She had fracture at right orbital floor, right multiple rib, posterior wall of right pelvis acetabulum, and right tibial plateau. Also, liver laceration, hemoperitoneum, and right posterior cruciate ligament partial tear was found. She received medication treatment, applied a cast to her right leg, and was hospitalized from July 13 to July 27. After she was discharged from the university hospital, she was hospitalized to another orthopedic hospital, and was taken MRI (C-spine, Elbow), and a fracture of olecranon process was found. She was hospitalized from July 27 to July 30 and then discharged, and visited our hospital for intensive Korean medicine treatment.
9. Current medication
1) Gastiren Tab . 1T qd pc ( July 30∼August 5).
2) Loxoprofen DKW Tab. 60mg 1T qd pc (July 30∼August 5).
3) SamChunDang Magnesium oxide Tab. 250 mg 1T qd pc (July 30∼August 4).
4) Carol-F Tab. 1T PRN (when pain is severe) : Carol-F Tab. was administered due to injured region pain on August 9, August 15, August 20, and August 22.
10. Review of system
1) Sleep: She slept for 7 hours a day before onset, but reduced to 5∼6 hours after onset. After the accident, when lying down at night, she complained of shrinking her hand.
2) Appetite and digestion: She had slight decrease in appetite since the onset. She also complained of persistent nausea and abdominal discomfort.
3) Defecation: She usually defecated loose stools and felt gassy.
4) Tongue diagnosis: Pale red tongue and thick white fur (淡紅 白厚苔).
5) Pulse diagnosis: Sunken and fine (沈細).
12. Korean medicine diagnosis
We diagnosed the symptoms as b lood deficiency (血虛), insufficiency of heart and gallbladder (心膽虛怯), and dual deficiency of the heart and spleen (心脾兩虛).
14. Treatment
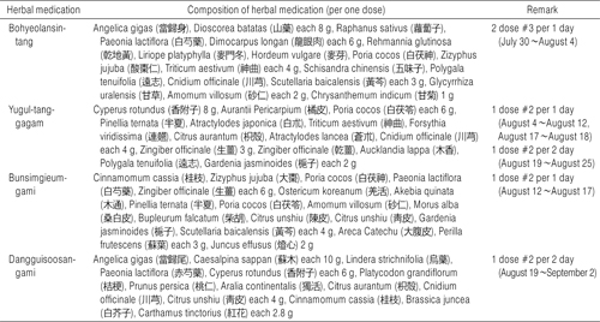
1) Herbal medicine (Table 1)
(1) Bohyeolansin-tang (補血安神湯) tid: From July 30 to August 4.
(2) Yugul-tang-gagam (六鬱湯加減) bid: From August 4 to August 12.
(3) Bunsimgieum-gami (分心氣飮加味) bid: From August 12 to August 17.
(4) Yugul-tang-gagam (六鬱湯加減) bid: From August 17 to August 18.
(5) Yugul-tang-gagam (六鬱湯加減) qd (at morning): From August 19 to August 25.
(6) Dangguisoosan-gami (當歸鬚散加味) qd (at evening): F rom August 19 to September 2.
2) Acupuncture
Acupuncture (0.30×30 mm disposable acupuncture needle; Dong Bang Acupuncture Factory) treatment was applied once a day. Left heart tonifying acupuncture (心正格; Toniyfing HT9 (少衝) and LR1 (大敦), sedating HT3 (少海) and KI10 (陰谷)), GV20 (百會), GB20 (風池), CV22 (天突), PC6 (內關), LU7 (列缺), HT7 (神門), ST36 (足三里) used as basic acupoints. According to the patient’s pain level, left liver tonifying acupuncture (肝正格; Tonifying LR8 (陰谷) and KI10 (曲泉), sedating LR4 (中封) and LU8 (經渠)), the right rib region, finger joint, neck, shoulder, and lower back were used as additional acupoints. Also, electroacupuncture was applied to the acupoints at the region of pain. Needle retention time was set at 15 minutes.
3) pharmacopuncture
Jungsongouhyul (中性瘀血) pharmacopuncture was injected into the area complaining of pain in the both arms, both legs, etc. twice a week.
4) Moxa
Indirect moxa (間接灸; Dong Bang Moxa Factory) was applied on a CV12 (中脘) and CV04 (關元) for 30 minutes once a day.
5) Cupping
Dry cupping treatment was applied on bilateral baesu-point (背兪穴) for 5 minutes once a day.
15. Instruments of evaluation
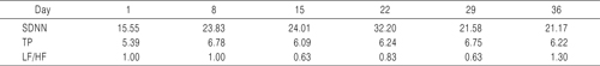
2) Heart Rate Variability (HRV) (Table 2)
Heart rate variability was measured in a quiet room in a supine position for 5 minutes once a week.
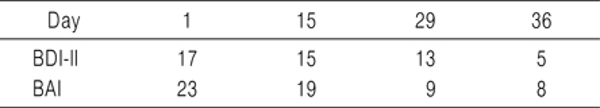
3) BDI (Beck Depression Inventory)-II, BAI (Beck Anxiety Inventory) (Table 3)
BDI-II consists of 21 questions and is composed of a likert scale of 0 to 3 points per question. It has a score range of 0 to 63 points, 14 to 19 points indicates ‘mild depression’, 20 to 28 points indicates ‘moderate depression’, and 29 to 63 indicates ‘severe depression’9).
BAI consists of 21 questions and is composed of a likert scale of 0 to 3 points per question. It has a score range of 0 to 63 points, 22 to 26 points indicates ‘anxiety state (requiring observation and intervention)’, 27 to 31 points indicates ‘severe anxiety state’, and 32 to 63 indicates ‘extremely anxiety state’10).
We assessed BDI-II and BAI on the first, 15, 29, and 36 days of hospitalization.
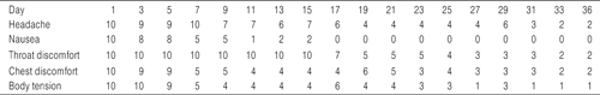
4) Global assessment (G/A) (Table 4)
Assuming that the level of symptoms the patient felt at the time of hospitalization was ‘10’ and when there was no pain as ‘0’, the degree of symptoms the patient-perceived after treatment was expressed in numb ers compared to those a t the time o f hospitalization.
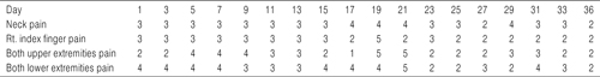
5) Numerical rating scale (NRS) (Table 5)
The degree of pain the patient felt was expressed as a number between ‘0’ and ‘10’. The degree of pain was measured in the neck, right index finger, both upper extremities, and both lower extremities.
16. Clinical course and outcome
1) Day 1∼Day 5
The patient was hospitalized in our hospital to receive Korean medical treatment after 18 days of acute treatment at western medical institutions. She complained of pain in the frontal and right head, and continued nausea and dizziness. She complained of a feeling of body tension intermittently, and she said that when she opened her mouth, she felt uncomfortable as it pulled from the neck to the shoulder. After the accident, she felt symptom of shrinking both hand when lying down. She said that the feeling of something filled around the throat during swallowing was even before the accident, but it got worse after the accident. At the time of inhalation, she complained of discomfort around the right rib. Sometimes she said that she kept thinking of the accident situation and complained of anxiety about returning to daily life. She sweats a lot during sleep and awakens several times for no other reason during sleep. She complained of neck pain, right index finger pain, both upper extremities pain, and both lower extremities pain, and were at the level of NRS 4. We prescribed bohyeolansin-tang (補血安神湯) and started acupuncture treatment. Until the 3rd day after hospitalization, the overall symptoms were slightly alleviated, but on the 4th day, the headache and neck discomfort became severe, and she could hardly sleep. The feeling of nausea also deepened to the level of the first day of hospitalization. Jieon-goron therapy (至言高論療法) was performed to support her who was anxious due to intensifying symptoms.
2) Day 6∼Day 13
Until the 6th day of hospitalization, somatic symptoms and pain were maintained at similar levels, but she complained of dyspepsia and abdominal pain at dawn, so she could not sleep well. So, we changed the prescription to yugul-tang-gagam (六鬱湯加減). She said it was difficult to take the herbal medicine 3 times a day, so we changed from taking 3 times a day to 2 times a day. On the 7th day of hospitalization, the next day after the prescription change, symptoms of dyspepsia including abdominal pain did not complain, nausea was relieved, body tension, and chest discomfort were greatly relieved. She said that the body seemed to relax after taking yugul-tang-gagam (六鬱湯加減). Neck pain and upper and lower extremity pain were maintained. From the 8th day of hospitalization, all of the western medicines (Gastiren Tab., Loxoprofen DKW Tab., and SamChunDang Magnesium oxide Tab. 250 mg) were exhausted and no longer taken. But, neck pain, upper and lower extremity pain that complained of after the traffic accident did not worsen. On the 10th day, the feeling of nausea that had been constantly appealing after hospitalization almost disappeared. On the 11th day, she complained of severe pain in the right lower extremity and took Carol-F tablet.
3) Day 14∼Day 18
While taking yugul-tang-gagam (六鬱湯加減) for about a week the dyspepsia symptoms improved, but she felt her body saggy. We was changed the prescription to bunsimgieum-gami (分心氣飮加味) on the 14th day of hospitalization. On the 15th day of hospitalization, she complained of fear due to somatic symptoms and anxiety that she might not be able to walk well even after the cast was removed. So jieon-goron therapy (至言高論療法) was performed to reassure her who was anxious due to intensifying symptoms. From the 16th day of hospitalization, the headache was alleviated to G/A 5, and the throat discomfort began to gradually relieve. From the 17th day of hospitalization, she no longer complained of nausea. On the afternoon of the 17th day of hospitalization, the pain in the right lower extremity became worse again, and she took Carol-F tablet again. Meanwhile, from the 14th day of hospitalization, the day she slept well for 6∼7 hours and the day could not sleep properly for 1∼2 hours continued to appear alternately.
4) Day 19∼Day 25
After taking bunsimgieum-gami (分心氣飮加味), her sleep became poor, and she said that it seemed to improve digestion when eating yugul-tang-gagam (六鬱湯加減) rather than bunsimgieum-gami (分心氣飮加味). From the 19th day of hospitalization, the prescription was changed to yugul-tang-gagam (六鬱湯加減) again. After the change of prescription, the symptoms of dyspepsia almost disappeared. However, at night, the pain in both upper and lower extremities intensified, making it difficult to sleep, and numbness in the cast area of the right lower extremity appeared. So the morning prescription was maintained as yugul-tang-gagam (六鬱湯加減), and only the evening prescription was changed to dangguisoosan-gami (當歸鬚散加味). After changing the evening prescription, she slept well within 6∼7 hours. Neck pain, right index finger pain, both upper and lower extremities pain, and chest discomfort also gradually decreased. From the 23rd day of hospitalization, she said that the body tension and the symptoms of shrinking both hands when lying down seem to alleviate little by little. She said that the pain in her right index finger intensified during the day, and the difficulty and range of motion (ROM) limitations were severe during the day. She took 1 Carol-F tablet each on the 22nd and 24th day of hospitalization. She also reported that from the 23rd day of hospitalization, pain around the lower back began to be felt.
5) Day 26∼Day 36
On the 26th day of hospitalization, she went to a university hospital to follow up. The cast was removed because the bones of the knee were well mended, and she was heard that it is okay to wear a knee protector only during activities and perform simple knee exercises. After the accident, she only moved in a wheelchair, but after removing the cast, she was able to move on crutches. However, her right leg to which the cast was applied for a long time was swollen, and some pain complained. We helped her, who was anxious, recognized and supported her as a process of gradually improving. On the 27th day of hospitalization, body tension and anxiety decreased, and discomfort in the throat and chest was also slightly relieved. She also said that she felt a little uncomfortable because he moved her right leg after a long time. Since she rarely complained of dyspepsia related symptoms, from the 28th day of hospitalization, yugul-tang-gagam (六鬱湯加減) was no longer administered in the morning, and the herbal medicine was taken only in the evening. The feeling of dullness in the head was maintained at G/A 4, and the throat and chest discomfort remained at G/A 3. She that the somatic symptoms, such as the upper limb shrinking when lying down, almost disappeared. She said that the right index finger pain, neck pain, and back pain still remain, and she was anxious if the pain sometimes gets worse. In addition, she said that while moving through crutches, she could not put his right leg on the ground, so she felt stiff pain in the left upper limb and armpit. At the dawn of the 29th day of hospitalization, the pain and headache around the right ribs intensified, and she could not sleep properly. So jieon-goron therapy (至言高論療法) was performed to relieve her anxiety of worsening of symptoms, and the pain relieved again from the 30th day of hospitalization. The overall pain tended to be relieved, but the tingling pain in the both upper extremities and the feeling of lumps were intermittently complained. In addition, she expressed that some pain was felt while performing a simple exercise of right knee. On the 31st day of hospitalization, she expressed her fear of the aftereffects that occurred after the accident and we informed her that the process was gradually improving through jieon-goron therapy (至言高論療法), and reassured her. Afterwards, somatic symptoms and pain remained at similar levels until discharge. Although the pain appeared intermittently at night, she did not take Carol-F tablet. She also said that the pain gradually decreased as the right knee exercise was repeated. The swelling of the right leg was also gradually relieved. On the 36th day, the last day of hospitalization, the degree of pain she complained was also improved compared to at the time of hospitalization. The neuropsychiatric treatment related to somatic symptom disorder was terminated, and in order to receive continuous treatment with the aim of controlling pain, she was discharged from our hospital and transferred to another Korean medicine hospital.
III. DISCUSSION
The number of traffic accident patients in Korean medicine has increased by 167% from 480,000 in 2014 to 127 million in 201911). However, the psychosomatic symptoms of the injured tend to be neglected compared to the physical symptoms. Somatic symptoms often are accompanied by psychological symptoms such as initial ‘shock’, a ‘dazed’ feeling, anxiety, anger, depression, difficulty concentrating, insomnia, lassitude, loss of libido, altered appetite and weight, and in some cases, feelings of helplessness, horror, despair and reliving experiences12). It is also affected by trauma characteristics, individual predisposition, and characteristics of the recovery environment13). This has the potential to be solved through the Korean medicine theory of ‘body and mind as one (心身一如)’.
Patients with somatic symptom disorder tend to show hypersensitivity to somatic sensations and have a low threshold for pain2). As a psychological factor, suppressed stress is converted into anxiety, frustration, or painful emotions or memories by using defense mechanisms such as repression, introjection, and somatization14). According to the social learning model, the use of the disease state as a reason to avoid social pressures, obligations, and unwanted situations is explained as learning through observation or indirect experience, and this is called a ‘sick role’3). Among patients with somatic symptom disorder, people with a neuroticism personality are common2).
For the treatment of patient with somatic symptom disorder, it is necessary to focus on managing stress and dealing with the process of adapting to chronic diseases. It is great to have a single doctor responsible for consistent treatment. Cognitive behavioral therapy, psychological therapy such as psychoanalysis, and behavioral therapy such as biofeedback can be helpful. Depending on the target symptoms, medication may be considered. In western medicine, anxiolytics such as benzodiazepine, antidepressants such as selective serotonin reuptake inhibitor may be used2,3,14).
According to epistemology of ‘body and mind as one (心身一如)’, excessive emotional changes are considered to cause diseases in the human body, and treatment according to the cause and pattern differentiation is performed15).
The patient in this case received acute treatment for 18 days at western medical institutions after the traffic accident, and then was hospitalized in our hospital to receive neuropsychiatric treatment for the somatic symptoms she complained of after the traffic accident.
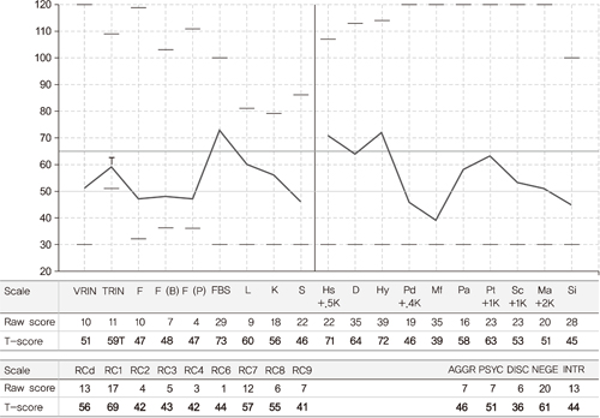
MMPI-2 was performed at the time of hospitalization to evaluate the patient’s psychological state, it was found that the Hy and Hs scales of the clinical scales was out of the normal range. As such, patients showing a 3-1 (Hy-Hs) upward scale pair are often diagnosed with somatic symptom disorder or pain disorder, and may report symptoms of anxiety and depression. They use denial, projection, rationalization defense mechanisms well, are unstable, and may have a desire to receive sympathy from others. In the validity scales, only the FBS scale was found to be out of the normal range. The FBS scale is a scale that detects the tendency to make false emotional pain (faking illness), but it also measures overall maladjustment and complaints of somatic discomfort. In the restructured clinical scales, RC1 was found to be out of the normal range. An increase of the score on the RC1 scale is associated with obsession with somatic health, somatic discomfort, depression and anxiety symptoms16).
The patient in this case was sensitive and under constant stress and complained of various somatic symptoms such as throat discomfort, chest discomfort, and whole body tension intermittently even before the traffic accident, and she had problems with her daily life because of these somatic symptoms. In addition, anxiety and fear about somatic symptoms affected her job activities, and even if the somatic symptoms did not persist, the state of being symptomatic was persisted for a long time. Referring to the DSM-5 diagnostic criteria, MMPI-2 results, and social history, we diagnosed her with a somatic symptom disorder.
At the time of hospitalization, the patient complained of anxiety, insomnia, headache, and dizziness, along with somatic symptoms. We diagnosed her symptoms as blood deficiency (血虛), insufficiency of heart and gallbladder (心膽虛怯). Bohyeolansin-tang (補血安神湯) was administered. Bohyeolansin-tang (補血安神湯) is a prescription based on samultang (四物湯) to have the effects of nourishing the blood (補血), calming nerve (安神), clearing heat (淸熱), relieving pain4). After administration of bohyeolansin-tang (補血安神湯), overall somatic symptoms and pain tended to be slightly relieved. But from the 4th day of hospitalization, somatic symptoms tended to worsen again, and symptoms of dyspepsia such as abdominal pain and nausea were intensified. We diagnosed her symptoms as qi movement stagnation(氣鬱) additionally and changed the prescription to yugul-tang-gagam (六鬱湯加減). To express the burden of the patient taking the herbal medicine 3 times a day, the number of administrations was changed to 2 times a day. Yugul-tang-gagam (六鬱湯加減) is used for talyoung (脫營), anxiety, and dyspepsia14). Nausea, body tension, and chest discomfort symptoms were greatly relieved while taking yugul-tang-gagam (六鬱湯加減) for about a week. However, even after taking yugul-tang-gagam (六鬱湯加減), the patient felt a lot of chest discomfort, so it was changed to bunsimgieum-gami (分心氣飮加味). Bunsimgieum-gami (分心氣飮加味) is used for nervous breakdowns, anorexia, eructation (曖氣), acid regurgitation (呑酸), nausea and other symptoms4). By administering bunsimgieum-gami (分心氣飮加味), we tried to improve the symptoms of dyspepsia, anxiety, throat discomfort, and chest discomfort that patient complained of. After the administration of bunsimgieum-gami (分心氣飮加味), the feeling of blockage in the throat began to gradually relieve, and the feeling of dullness in the head was also slightly relieved. However, while taking bunsimgieum-gami (分心氣飮加味), insomnia occurred intermittently and the patient seems to have a worsening of dyspepsia symptoms, so we rechanged the prescription as yugul-tang-gagam (六鬱湯加減). Afterwards, the prescription was changed again to take yugul-tang-gagam (六鬱湯加減) only in the morning and in the evening to take dangguisoosan-gami (當歸鬚散加味) for the improvement of upper limb pain that the patient complained of at night. Dangguisoosan-gami (當歸鬚散加味) is a prescription that is widely used for static blood (瘀血) due to trauma17). After the administration of dangguisoosan-gami (當歸鬚散加味), the pain in the neck, right index finger, as well as upper extremity, which mainly complained at night, gradually decreased. Insomnia was also improved. In addition, as the degree of pain decreased, the anxiety and somatic symptoms complained of by the patient tended to improve together, and dangguisoosan-gami (當歸鬚散加味) was prescribed continuously until discharge.
The acupuncture combination used in this study, heart tonifying acupuncture (心正格; Tonifying HT9 (少衝) and LR1 (大敦), sedating HT3 (少海) and KI10 (陰谷)), has the effect of treating heart deficiency (心虛) and mental disorders18). Acupoints such as GV20 (百會), CV22 (天突), PC6 (內關), HT7 (神門), and ST36 (足三里) were used to relieve psychological anxiety and somatic symptoms such as throat discomfort and chest discomfort. Meanwhile, liver tonifying acupuncture (肝正格; Tonifying LR8 (陰谷) and KI10 (曲泉), sedating LR4 (中封) and LU8 (經渠)) has the effect of relieving liver stagnation (肝鬱). In addition, there have been a number of studies reported on the control of pain such as cervical pain, lumbar pain, and neuralgia of the liver tonifying acupuncture19). Jungsongouhyul (中性瘀血) pharmacopuncture was administered twice a week. Jungsongouhyul pharmacopuncture is used for pain or paralysis disease caused by qi stagnation and blood stasis (氣滯血瘀)17). The above acupuncture treatment is thought to have led to the effect of improving the somatic symptoms and pain that patient complained of.
The patient complained of various somatic symptoms intermittently before the accident. After the accident, the somatic symptoms became worsen, and she complained of pain in various parts of the body. During hospitalization, the Global Assessment (G/A) was used to determine the degree of improvement in somatic symptoms, and the Numerical Rating Scale (NRS) was used to determine the degree of pain improvement. Comparing the G/A and NRS for each symptom on the first and last days of hospitalization, it was found that the degree of symptoms decreased in most of the symptoms, leading to improvement in symptoms.
At the time of hospitalization, the patient was in a mild depressive state with 17 points on the BDI-II, and an anxiety state with 23 points on the BAI. BDI-II and BAI were performed at intervals of 2 weeks, and the scores showed a tendency to gradually decrease with each application. On the discharge date, BDI-II score was 5 and BAI score was 8, which were all in the normal category. This improvement in BDI-II and BAI scores indicates that the patient’s depression and anxiety have been resolved after hospitalization treatment, and it can be predicted that the prognosis of her somatic symptoms after the traffic accident will be positive.
Since somatic symptoms in somatic symptom disorder are related to stress and autonomic nervous system dysfunction21), the heart rate variability was performed at 1 week intervals to evaluate the level of stress felt by the patient and the balance of autonomic nervous system. Among the results of heart rate variability, changes in SDNN, TP, and LF/HF ratio values were observed. SDNN (standard deviation of all normal R-R intervals) indicates the complexity of the heart rate variability. Healthy people have high SDNN due to large heart rate variability. But in disease or stress situations, SDNN is low due to small heart rate variability. TP (Total power) refers to the activity of the entire frequency domain and reflects the overall activity and flexibility of the autonomic nervous system. LF (Low Frequency Power) is related to both sympathetic and parasympathetic nerves, and HF (High Frequency Power) represents parasympathetic activity. The LF/HF ratio means the control and balance of the heart’s parasympathetic and sympathetic nerves. The ideal value is 1.5∼2.022). In the HRV test performed at the time of hospitalization, SDNN was 15.55, TP was 5.39, and LF/HF was 1.00. The SDNN at the time of discharge was 21.17, which was higher than the SDNN at the time of hospitalization of 15.55. However, until the 3rd week of hospitalization, the SDNN tended to increase gradually, but from the 4th week of admission, the SDNN tended to decrease. TP rose and fell repeatedly. LF/HF was 1.30 at the time of discharge, which was relatively close to the ideal value of 1.5 to 2.0. As a result, it can be seen that the balance ratio of the patient’s autonomic nerve is close to the normal range at the time of discharge, but the degree of stress felt by the patient is somewhat high. Significant improvement in somatic symptoms and pain was shown, and HRV results did not significantly improve at discharge even though BDI-II and BAI scores were lowered. As the discharge date approaches, it is thought that it is because of the fear of returning to work after discharge.
In this case, a patient with a somatic symptom disorder who was hospitalized to a Korean medicine hospital after traffic accident was treated with Korean medicine treatment such as herbal medicine, acupuncture treatment, and psychotherapy for 36 days. It is thought to be meaningful in that it had a significant effect on improving anxiety, somatic symptoms, and pain level. The limitations of this study are that there was only one patient case, that western medicine therapy was combined, and that the progress was evaluated mainly by subjective evaluation of patient such as NRS and G/A. Somatic symptom disorder is difficult to treat and often shows a chronic course, so it is thought that more attention and research on somatic symptomatic disorder is needed. We look forward to the publication of case reports and control studies on more diverse somatic symptom disorders in the future.