
Critical Success Factors for the Adoption of Health Management Information Systems in Public Hospitals in Zimbabwe
Indira Padayachee (School of Management, IT and Governance, University of KwaZulu- Natal, Durban, South Africa)
Abstract
The Zimbabwean healthcare sector faces huge challenges due to increased demands for improved services for a growing number of patients with fewer resources. The use of information and communications technologies, prevalent in many industries, but lacking in Zimbabwean healthcare, could increase productivity and innovation. The adoption of health management information systems (HMISs) can lead to improved patient safety and high-level patient care. These technologies can change delivery methods to be more patient focused by utilising integrated models and allowing for a continuum of care across healthcare providers. However, implementation of these technologies in the health care sector remains low. The purpose of this study is to demonstrate the advantages to be attained by using HMISs in healthcare delivery and to ascertain the factors that influence the uptake of such systems in the public healthcare sector. A conceptual model, extending the technology, organization, and environment framework by means of other adoption models, underpins the study of adoption behavior. A mixed method methodology was used to conduct the study. For the quantitative approach, questionnaires were used to allow for regression analysis. For the qualitative approach, thematic analysis was used to analyse interview data. The results showed that the critical success factors (namely, relative advantage, availability, complexity, compatibility, trialability, observability, management support, information and communication technology expertise, communication processes, government regulation, infrastructure support, organizational readiness, industry and competitive support, external support, perceived ease of use, perceived usefulness, attitude, and intention to use) influenced adoption of HMISs in public hospitals in Zimbabwe.
- keywords
- health management information systems, technological factors, organizational factors, environmental factors, individual factors, technology, organization, and environment framework
1. INTRODUCTION
Information and communication technologies (ICTs) have been applied in various industries for the collection, editing, transmission, and storage of information to improve service delivery. They aid organizational members in communicating, cooperating, and collaborating freely by removing the challenges of distance and time (Bacigalupe, 2011). This trend also occurs in health delivery institutions as they search for ways to improve service delivery, with one such innovation being the health management information system (HMIS). The main goal of incorporating information technology (IT) into the healthcare industry is improving patient care procedures already in existence and introducing new and innovative capabilities by removing the disadvantages of limited opening times, queues, paperwork, travel, and other challenges inherent in the old means of service provision. The use of HMISs has the potential to improve patient outcomes, while at the same time lowering costs.
1.1. Health Management Information System
An HMIS is designed to manage healthcare data by collecting, storing, manipulating, and transmitting patient data, by helping with hospital operational management and by supporting healthcare policy decisions at community, district, provincial, and national levels (Ariani et al., 2017). HMISs are critical in unifying communications through fully integrated audio-visual data communications and electronic systems. The architecture of an HMIS comprises three key levels of use and aggregation, namely, the patient-carrying level, the territory level, and the central government level. The patient level carries information about a patient’s medical history, whilst the territory and government levels carry aggregated information about the medical staff, departments, operations, and management policies, as well as other decision-making related information (Asemahagn, 2017).
A good HMIS should provide relevant information that shows where service is lacking and should highlight the intervention needed in such areas. It should also allow access to reliable, timely, and authorised data by all relevant people, including partners, for implementation of different programs that will improve the healthcare (Chatterjee, 2015). Information is considered an indispensable operational asset necessary for effective management and development of health services; hence the need for an HMIS to support management at all levels (Alwan et al., 2015). The result of using an HMIS will be quality, cost effective, and efficient healthcare services for all (Asemahagn, 2017).
The adoption of HMISs in Zimbabwe would provide horizontal and vertical linkages of health systems such that patient data can be shared across all health systems with the aim of providing improved healthcare to patients. It should encompass all the aspects of healthcare, such as patient data storage, management of healthcare, and allocation of resources. Typically, an HMIS comprises various subsystems such as billing, intensive care unit systems, outpatients, maternity, drug inventory, duty allocations, and many others and should be accessible throughout the whole healthcare system.
1.2. Public Health System in Zimbabwe
In Zimbabwe, the largest proportion of healthcare services is accessed through the public health system and supplemented by mission hospitals and sometimes by non-governmental organizations. The health delivery system in Zimbabwe is divided into a four-level structure: primary, secondary, tertiary, and quaternary. The primary level, known as primary healthcare, drives most of the healthcare programmes such as the essential drugs programme, expanded immunisation, communicable disease control, curative and essential preventive services, food production and nutrition education, health education, and maternal and child services (Ministry of Health and Child Welfare, 2009).
According to official studies such as the Zimbabwe Maternal and Perinatal Mortality study of 2007, the Zimbabwe Demographic and Health Survey of 2005/2006, and the Multiple Indicator Monitoring Survey of 2009, the Zimbabwean populace is succumbing to diseases that can easily be prevented or treated, such as diarrhoea, Human immunodeficiency virus (HIV) and tuberculosis (TB)-related illnesses, malaria, malnutrition, and injuries, and in most cases, deaths are recorded in unusually high numbers. The management and treatment of patients suffering from such illnesses and other chronic diseases takes place over a lengthy period and is carried out by different healthcare providers in different settings. To achieve higher quality and safety in the delivery of healthcare, information should be presented in a structured manner, ready for use in clinical decision making, which can be achieved with the implementation of HMISs that support online access to health records, secure transmission of medical information between systems, and shared longitudinal electronic health records (RTI International, 2014).
The current system from facility to district health information is paper based, becoming computer based on provincial health information to national health information (United Nations Development Programme [UNDP], 2014b), and as such there is little support for accessibility to health consumer information. Attempts at computerisation in Zimbabwe have seen the development of various systems targeted at specific programmes, diseases, or areas. The systems are not integrated, nor do they cover the entire healthcare continuum of patients, thus allowing for a national picture of healthcare provision. Starting in 1985, a Microsoft Access based system was commissioned by the Ministry of Health and Child Care (MoHCC) to collect and report on routine data, but it soon became slower and less efficient. From 2011 to 2012, the country implemented the District Health Information Software version 1.4 (DHIS1). In 2012 the MoHCC got help from The United States President’s Emergency Plan for AIDS Relief (PEPFAR) to pilot a DHIS-2 in Manicaland, and was scaled to other provinces in 2013 with the help of funding from UNDP, PEPFAR, and other partners (UNDP, 2020). Another system of note is the FrontlineSMS system launched by the MoHCC, a mobile-phone-based system used for transmitting early infant diagnosis of HIV from selected health facilities to the Zimbabwe’s National Microbiology Reference Laboratory.
In 2012 the government, through the MoHCC and in partnership with various donor agencies such as World Health Organization (WHO), UNDP, Joint United Nations Programme on HIV/AIDS, the National AIDS Council, Centre for Disease Control, and the Research Triangle Institute, started piloting an electronic patient management system for HIV and TB. The first phase began in 2013, with the system installed at 85 sites and covering 65% of all national patients; 161 more sites were added in 2014, taking the total to 246. The plan was to implement Phase 3 of the project between 2015 and 2016, adding the remaining 184 facilities and bringing the number of patients covered to 97% (UNDP, 2014a). At Chitungwiza Hospital, a system using the System Applications and Products in Data Processing (SAP) Health Software application had approximately 100 desktop computers in all departments and wards, and these were used as access points. The system was linked to a central server at MoHCC headquarters with a fast fibre-optic link. Members were given login details to access the system. The system was used for tasks such as clinical information storage, capture of patient demographic data, and handling accounts of patients (Techzim, 2014).
1.3. Problem Statement
Challenges with regard to the old manual and current systems include difficulties in maintaining manual records and in the preparing and sharing of reports, a lack of standard names and codes to be used in service delivery, difficulty in monitoring and evaluation of hospital performance without real-time data, and a lack of adequate data to perform evidence-based program management (Asemahagn, 2017; Tan, 2009). The need to have HMISs in hospitals is driven by the growing need for connectivity among healthcare providers, for patients to participate in their personal care, for the managing of market pressures associated with healthcare provision, and for exploiting the great improvements in IT that have improved systems interoperability (International Center for AIDS Care and Treatment Programs at Columbia University, 2015; Tan, 2009). The challenges being experienced with old technologies such as tapes and folders is now pushing executives and healthcare givers to consider the implementation of innovative HMISs to improve healthcare delivery (Herrick et al., 2010; Ross & Venkatesh, 2016).
Though the benefits of using HMISs are known, few studies have dealt with the critical success factors (CSFs) for their adoption in Zimbabwe. The ICT infrastructure has developed to an extent where it is possible to computerize some or all of the repetitive information processing in hospitals and to meet the required information standards in minimal time with less effort on the part of staff, patients, and healthcare professionals. The opportunity to access health care information, including patient hospital records, which is fundamental to the delivery of healthcare services, has been hampered by a lack of suitable information systems. Studies documenting the issues around the adoption of HMIS in healthcare institutions in Zimbabwe are not available. Proper evaluations and proof regarding the perceived benefits and challenges to adoption in Zimbabwe are generally lacking.
The goal of this research study is to ascertain the CSFs that drive the adoption of an HMIS in Zimbabwe. The factors from the technology, organization, and environment (TOE) theory are used with additional constructs from other organizational and individual theories, such as the diffusion of innovation (DOI) theory, theory of reasoned behavior (TRB), theory of reasoned action (TRA), and the technology acceptance model (TAM), in order to construct a modified theoretical framework for explaining the CSFs influencing the adoption of HMISs at the organizational level.
1.4. Theoretical Framework
The main theory underlying this study is the TOE model, modified with constructs from other adoption models. The TOE framework is the work of Tornatzky and Fleischer (1990) and depicts the process a firm goes through during the adoption and implementation of technological innovations in the context of technological, organizational, and environmental factors. The internal and external technologies available and relevant to a firm constitute the technological context. The resources available and the internal characteristics of the organization constitute the organizational context. The industry’s structure and size, the existing competition to the firm, the macroeconomic environment, and the regulatory framework and environment is what constitutes the environmental context (Tornatzky & Fleischer, 1990).
The TRA posits that an individual’s behavior is a function of their intention, which in turn is a function of their attitude and subjective norms (Fishbein & Ajzen, 1975).
The theory of planned behavior (TPB) by Ajzen (1985) is similar to the TRA as it shows the link between an individual’s behavior as influenced by intention, which in turn is a function of attitude, subjective norms, and perceived behavioral control (PCB).
The TAM by Davis (1989) has been widely used and accepted in adoption studies and it explains how perceived ease of use (PEOU) and perceived usefulness (PU) are regarded as the primary factors influencing an individual’s intention to use a new innovation.
The TAM2 developed by Venkatesh and Davis (2000) is an extension of the TAM model and incorporates additional constructs, namely social influence and cognitive instrumental processes. TAM2 uses subjective norm, voluntariness, and image as the three interrelated social forms in determining whether an individual will accept or reject a new innovation.
The DOI theory from the work of Rogers (1962) states that different people in a society will not adopt an innovation uniformly but will do so at different times and stages. Rogers (1962) identifies the five main factors responsible for affecting the adoption of an innovation as relative advantage, compatibility, complexity, trialability, and observability, which have a different extent of influence in the five adopter categories. These are the five factors used from DOI to assess the technological category in the next section on conceptual framework and constructs.
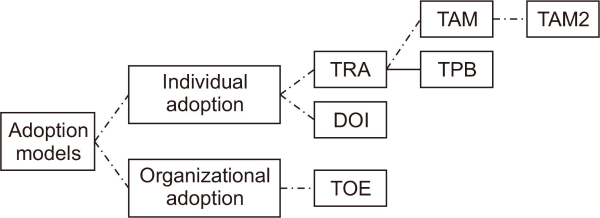
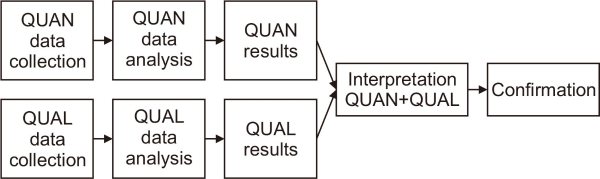
The relationships between the models used are shown in Fig. 1.
Fig. 1
Relationships between adoption models. TRA, theory of reasoned action; DOI, diffusion of innovation; TOE, technology, organization, and environment; TAM, technology acceptance model; TPB, theory of planned behavior.
1.5. Conceptual Framework and Constructs
The main research aim of this study was to find the technological, organizational, environmental, and individual factors that are critical for the successful adoption of HMISs in Zimbabwean healthcare institutions. Appropriate research constructs validated in prior studies were borrowed from the literature and used for questionnaire development.
The TOE model by Tornatzky and Fleischer (1990) was adapted to determine the factors influencing adoption of IT innovations at the organizational level. While numerous studies have used the model with varying modifications to explain how organizations adopt technology, not all the modifications have been related to the health industry or have included individual behavioral models such as TPB and TRA. To bridge this knowledge gap, the TOE model was integrated with individual behavioral models, and additional constructs, such as attitude (TRA), intention to use, PEOU (TAM), and PU (TAM), to get a better understanding of the dynamics of technological adoption in healthcare institutions. The constructs to be operationalized and measured are provided in Table 1.
Table 1
Conceptual framework constructs
| Construct | Definition |
|---|---|
| Organizational | |
| Communication processes | The communication channels and how information flows in an organization (TOE) |
| Size | The larger the firm, the better the chances of surviving failures of new innovations (TOE) |
| Management support | Top management responsibility for cultivating the vision of the organization and encouraging success of technological innovation (TOE) |
| Organizational readiness | The availability of resources to allow for adoption of the said technology (TOE) |
| ICT expertise | The experience of the organizational members with ICT innovations |
| Technological | |
| Availability | How easily the required technology can be acquired (TOE) |
| Relative advantage | How an innovation is better compared to current practices (DOI) |
| Compatibility | How the innovation will match with the current systems and culture (DOI) |
| Complexity | How difficult it is to integrate and learn the new innovation for use if adopted (DOI) |
| Trialability | How easy it is to experiment with an innovation (DOI) |
| Observability | How easy it is to prove or show the results of an innovation (DOI) |
| Environmental | |
| External support | Other policy influences by external supporters to the organization and availability of support for implementation of the technology (TOE) |
| Technology infrastructure Support | The availability of the requisite infrastructure to support the use of the intended technology (TOE) |
| Government regulation | Government policies on use of the intended technology (TOE) |
| Industry and competitive pressure | Type of industry and competition that influences technological adoption (TOE) |
| Market scope | The market being served (TOE) |
| Behavioral/individual | |
| Perceived ease of use | The degree to which someone believes it is easy to learn to use the application (TAM/TAM2) |
| Perceived usefulness | The degree to which someone believes how important the use of the applications is and what the perceived benefits are, i.e., how it will enhance one’s work (TAM/TAM2) |
| Attitude | Negative or positive feeling about the decision to use an application (TRA) |
| Intention to use | A person’s readiness to adopt ICT innovations (TRB) |
The focus of this research is therefore to test the relationships among the constructs of HMIS adoption in the context of technology, organization, environment, and individual characteristics. In the investigation of technological, organizational, environmental, and individual factors affecting the adoption of HMIS by health institutions, 21 constructs were used in order to extend the existing knowledge base of technology adoption.
1.6. Research Questions
The specific research questions that are addressed in this article are as follows:
-
What are the organizational factors that influence the adoption of HMIS in Zimbabwean healthcare institutions?
-
What are the environmental factors that influence the adoption of HMIS in Zimbabwean healthcare institutions?
-
What are the technological factors that influence the adoption of HMIS in Zimbabwean healthcare institutions?
-
What are the individual factors influencing the adoption of HMIS in Zimbabwean healthcare institutions?
-
How can the CSFs be integrated into an adoption model for HMIS in public health institutions in Zimbabwe?
1.7. Research Model and Hypotheses
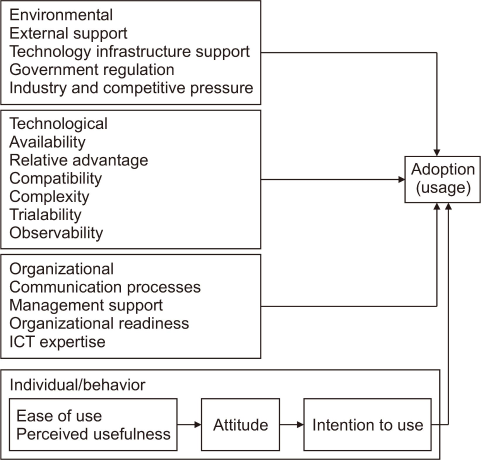
The model was derived from the combination of TOE, DOI, TRA, TPB, TAM, and other adoption models and was tested for relevance and confirmation in public health provision settings. The model and hypotheses are shown in Fig. 2.
Fig. 2
Research model and hypotheses: H1, Environmental factors influence technological decision making on adoption; H2, Technological factors influence technological decision making on adoption; H3, Organizational factors influence technological decision making on adoption; H4, Individual factors influence technological decision making on adoption; H5, Technological decision making on adoption influences adoption. ICT, information and communication technology.
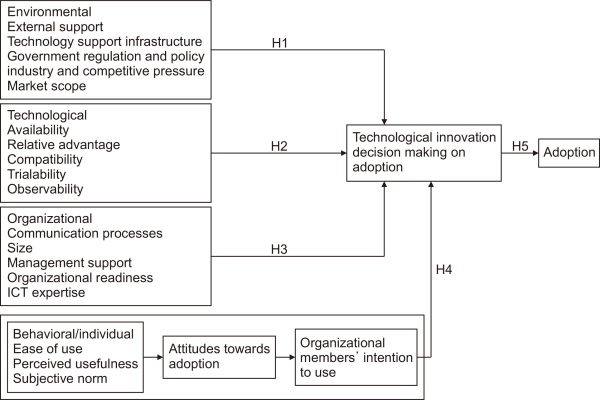
Hypotheses 1-3 are direct derivatives of the original TOE model with additional constructs from DOI; hypothesis 4 is an addition, adapted from the mixture of TOE and technology acceptance theories (TRA, TPB, TAM, TAM2), and H5 is from the TOE model.
-
H1. Environmental factors influence technological decision making on adoption.
-
H2. Technological factors influence technological decision making on adoption.
-
H3. Organizational factors influence technological decision making on adoption.
-
H4. Individual factors influence technological decision making on adoption.
-
H5. Technological decision making on adoption influences adoption.
2. RELATED MATERIALS
This section presents a literature review of factors that influence the adoption of information systems in the healthcare sector. Understanding the factors that influence the adoption of innovations and new ideas enables efficient dissemination of potential innovations. The decision to adopt an innovation is an engaging, interactive, and dynamic process that can be influenced by various individual, technological, environmental, and organizational factors. Alam et al. (2016) has concluded that organizational, technological, environmental, and human factors are responsible for the adoption pattern of a human resource information system in Bangladesh hospitals.
Technological factors are regarded as the characteristics of the existing technology and the proposed innovations that affect the adoption decision in an organization. Relative advantage refers to whether the technological innovation is better than the one it is replacing. It has been found to be important in the adoption of various health related information systems, e.g., in the study conducted by Hung et al. (2010) on customer relationship management in hospitals and that by Proscoviour (2017) on HMIS adoption in hospitals. Compatibility shows the extent to which the new system will operate with the current technology and fit into the organizational culture and processes. A study by Khobi et al. (2020) of DHIS2 adoption in Uganda, one by Marsan and Paré (2013) of adoption of open system software (OSS), and one by Proscoviour (2017) of HMIS adoption in Kenya all found compatibility to be important for the adoption of health-related systems. Eger et al. (2001) concurred that the amount of change needed to use the technology affects the adoption of ICTs by physicians; this factor was listed as a system interoperability issue by Kralewski et al. (2008). Complexity is the measure of how difficult it is to integrate and learn to use a newly adopted innovation. Complexity was found to be an important technological factor by Khobi et al. (2020) and by Proscoviour (2017).
Trialability, which refers to the opportunity for potential users to test the application before actual installation in the organization, has been found to be important for the adoption of innovations (Rogers, 1962). This technological construct was included in the study by Marsan and Paré (2013) but proved to be insignificant. Included in the same study was the construct of observability, which relates to how easy it is to show the results of an innovation and can be a measure of the popularity and use of the innovation in the industry. However, observability was reported to be insignificant for innovation adoption in this study. Availability relates to how easily the required technology can be acquired, involving the organizational availability of funds and the availability of the innovation at reasonable and affordable prices. Availability was used as an antecedent in the study by Dolan et al. (2020) and was given as the availability of electricity and the Internet in adoption of e-immunisation registries. Njeri (2018) used affordability in a study of adoption of HMIS, and Dixon and Dixon (1994) used availability of tools in their study of adoption decisions by physicians.
Organizational factors include the attributes of the organization and the resources it has available in its quest to adopt an innovation. Management support refers to management activities that influence the adoption of an innovation. Top management is responsible for cultivating the vision of the organization and encouraging success in the adoption processes. It was used as an antecedent by Khobi et al. (2020) and specified as the innovativeness of senior executives by Hung et al. (2010), and as support from management by Ifinedo (2018). These studies show that management support is important for adoption of innovation decisions. Communication processes represent the channels and mediums used within an organization and how they can potentially affect the adoption decision. Communication channels and information flow in an organization influence the type, rate, and success of innovation adoption in an organization. Dolan et al. (2020) used this factor in their studies and termed it as engagement among partners. Zhou et al. (2019) used this construct as interaction within communities in the organization, and found it to be important. Wang et al. (2005) used two constructs related to communication processes, that is, information processing and communication channels. Organizational size is a construct representing the influence of size on adoption decisions. It has been used in many studies and has been interpreted to mean that the larger the firm, the better the chance of surviving failures in an adoption process. The construct was used by Hung et al. (2010), who called it the size of the organization, and by Zhang et al. (2013), who used the number of beds to determine the size of hospitals. Both these studies concluded that size was important for the adoption of health-related innovative systems.
ICT expertise is a construct that defines the experience of the organizational members with ICT, and many studies have examined the influence of ICT expertise on the decision to adopt an ICT innovation. Marsan and Paré (2013) used the term for technological skills and knowledge, while Hung et al. (2010) listed it as IT capabilities of staff. Dixon and Dixon (1994) referred to it as the capabilities of the physicians in using the technology. These studies highlight the importance of ICT expertise in the adoption of innovations. Organizational readiness refers to the general preparedness of the organization to adopt an innovation and looks at the availability of resources (human, capital, and technology) in the organization and how they affect the adoption decision. Khobi et al. (2020) refer to ICT expertise as technology readiness, Proscoviour (2017) as organizational readiness, and Eger et al. (2001) as computer readiness. Organizational readiness covers all organizational resources that can affect the adoption of an innovation and has been shown to be an important antecedent in the studies mentioned above.
The environmental factor category is made up of all factors external to the organization but which have a bearing on its operations, and it has been indicated as a contributory factor in innovation adoption decisions. External support is one of the factors in this category, which refers to policy influences exerted on the organization by external supporters or the availability of IT support from outside organizations. The availability of external support tends to influence the adoption of ICT innovations positively. Ross et al. (2016) concluded that external support may facilitate adoption of technology and that it can be offered in the form of incentives by government or any other external stakeholder. Incentives could be financial and may be in the form of start-up funds to cover initial costs, financial sponsorship packages, compensations for adoption, and pay-for-performance initiatives. Marsan and Paré (2013) showed that external support is important when they used the construct of availability of external OSS expertise for the adoption of OSS by physicians. Alam et al. (2016) has used the construct of technology vendor support, which partly refers to external support, and this has proved to be a significant predictor of innovation adoption.
Technology infrastructure support refers to the availability of the requisite infrastructure to allow for the implementation and use of the intended technological innovation. Ross et al. (2016) note that many authors agree that availability of resources affects the decision to adopt and implement ICT innovations. Infrastructure includes access to computers, electricity supply, available bandwidth, reliable Internet connectivity, and access to phone lines and mobile phones. Park and Lee (2014) reported that small hospitals showed a more positive correlation between adoption of electronic medical records and a fully installed IT infrastructure than any other type of hospital.
Government regulation refers to government policies and influence on the use of the new technology. Ross et al. (2016) noted in their review of the literature that the shortcomings of legislature, policies, and standards can possibly derail the implementation of health information systems at any level, be it professional or organizational. Industry and competitive pressure refer to the type of industry and the pressure it can exert on an organization to adopt ICT. As noted by El Kandri (2018), the healthcare industry is generally under the control of governments, and hence there is no competition and no motivation to innovate and improve patient experience. The role of government is blamed for the lack of resources needed for the adoption of innovations due to constrained budgets, in contrast with countries where health care is controlled by the private sector and where there is more innovation. Market scope refers to the market being served and the influences it can have on the readiness of an organization to adopt an ICT innovation. Miraz and Habib (2016) found that the connection between market scope and adoption of ICTs is significant when they showed that the activities of the market, such as partner or customer adoption trends, can influence an organization to adopt.
The individual factor category describes factors that pertain to the behavior of an individual or a collection of individuals and how they influence the adoption of innovation in an organization. PEOU is an individual’s perception and belief regarding how easy it is for someone to learn to use an application; it is a measure of the effort required to be able to use the application. Ease of use is regarded as one of the factors in users’ adoption of new technologies. PU is a measure of how the new technology will enhance one’s work if adopted. It is a measure of how the innovation is better than the technology it succeeds. Although referring to studies outside of the health sector, Wanyoike et al. (2012) found a positive correlation between PU and an enterprise’s intention to adopt new Internet technologies. Attitude is the negative or positive feeling about the decision to use an application. Khan and Woosley (2011) stated that the main themes that emerged in their study of the literature regarding models that fit adoption in the health sector were attitude, efficiency of use, and usability, which were covered in TAM, DOI, and Unified Theory of Acceptance and Use of Technology. Their conclusion is that by understanding the attitudes and satisfaction of the physicians, the adoption of health IT can be increased.
Intention is a person’s readiness to adopt an innovation and the actions he or she makes to signal readiness to use an application. Macharia and Maroa (2014) in their study of adoption of HMIS in Kenya’s private hospitals concluded that behavioral intention has a significant role in predicting the usage of new innovations. Christodoulakis et al. (2017) listed the most notable barrier to adoption of remote patient monitoring technologies as the lack of user acceptance and their behavioral intention to adopt. The same study, however, indicated that the lack of adoption of electronic patient records was due to poor design of the application, inadequate use by clinicians, and socio-organizational factors such as lack of support from colleagues, which was supported by Khan and Woosley (2011). The constructs of PEOU and PU were found to have a significant influence on user intentions and behaviors in the adoption of cloud technologies in public service organizations using TAM (Shin, 2013).
Furusa and Coleman (2018) carried out a study on the elements influencing adoption of e-health and its implementation by public hospital medical doctors in Zimbabwe. The results showed that adoption and implementation of e-health was largely motivated by internal and external elements. The internal factors reported to be significant influencers were technical support, ICT infrastructure, security concerns, ICT skills and knowledge, refusal to accept change, practitioner-patient relationships, basic medical facilities shortages, and demographic data such as age. The external factors found to be significant influencers were funding, bureaucracy, and health policy.
However, most of the studies have been carried out in other regions and not in Zimbabwe, and are limited to enumerating the systems in use, accompanied by benefits, challenges, and implementation strategies of HMISs (Mapesa, 2016; RTI International, 2021; UNDP, 2014a; 2014b). The factors from the various studies, although using different approaches, frameworks, and methodologies, and in some instances being referred to by different names, can be grouped into a set of encompassing categories. This article reports on the synthesis of factors from the various adoption models to come up with a modified theoretical model to explain the adoption of HMISs in Zimbabwe, which could be used as a basis for carrying out similar studies in other regions.
3 METHODOLOGY
3.1. Research Approach
The mixed methods (pragmatic) researchapproach was used for the empirical study. It is a methodology that uses both quantitative and qualitative research techniques in one study (Creswell, 2014). Quantitative and qualitative methods were used concurrently for collecting both forms of data, labelled as the parallel-databases variant. The data from the two methods were kept distinct, that is, the data collection and analysis for the two approaches were done independently, and only combined at the interpretation stage, where the results were given equal priority in drawing conclusions. The collection and analysis of both sets of data occurred at approximately the same time.
The researcher compared the results for convergence during the interpretation stage. Where divergent results were obtained in quantitative and qualitative findings, the researcher considered the potential complementarity and completeness of the findings. Confirmation of findings was addressed in a later phase of the study by use of a third set of data collected to evaluate the model developed after the first two sets of data collection and analysis. The approach is depicted in Fig. 3.
Fig. 3
Convergence model of mixed method data analysis for the study. QUAN, quantitative; QUAL, qualitative. Adapted from Creswell, 2014. Research design: Qualitative, quantitative, and mixed methods approaches (4th ed.). Sage Publications.
3.2. Phase 1: Quantitative Data Collection and Analysis
This phase discusses the sampling, data collection, and data analysis of the quantitative data collected using the CSF questionnaire.
3.2.1. Target Population
The target population included those who work in various capacities in these health centres, such as the administrators, nurses, and doctors. The province has a population of about 1,486,604, as reported by 2012 Zimstat online ( https://www.zimstat.co.zw/). There is a physician density of 0.16, nurse density of 0.72, and an overall density of 1.23 health staff per 1,000 population in Zimbabwe. According to the WHO, density=population/workers, which in this study gives an estimate of 1,829 health workers comprising the target population for the province.
3.2.4.1. Factor analysis.
Factor analysis allows for the reduction of many variables to a smaller number of factors. The assumption is that the set of variables have not been measured perfectly. A factor is the name given to the unobserved or latent variables that make up common variance; thus, the test is named factor analysis (Garth, 2008). Factor analysis, more properly termed exploratory factor analysis, provides a mechanism for explaining the relationships of observed variables x1, x2, …, xn using a few unobservable factors, commonly referred to as common factors or latent variables f1, f2, …, fm where m<n and preferably is much less (Landau & Everitt, 2004). Factor analysis was performed first in the study to validate which factors were important in the adoption of HMISs.
3.2.4.2. Regression analysis.
Regression analysis technique provides an estimation of relationships between two variables, with one known as the dependent variable (DV) and the other as the independent variable (IV), and would be useful for modelling future relationships as well (De Smith, 2015). Regression analysis provides a reliable way to identify which variables have an impact on a subject under investigation. Carrying out regression analysis allows one to identify the important factors and their influence on the subject under study. This test was performed on the CSF questionnaire using the IBM SPSS Statistics version 20.0 (IBM Co., Armonk, NY, USA).
3.2.2. Sampling
A combination of convenience and random sampling was employed. Three hospitals were conveniently selected, and the participants were then randomly selected for the CSF questionnaire. The hospitals include Masvingo general hospital, Chivi District hospital, and Mogenster mission hospital in Masvingo Province. The questionnaires were distributed to the employees of the selected institutions until the target was reached, using systematic random sampling. Each institution was allocated the same number of questionnaires. The sample for the study comprised 360 participants.
3.2.3. Quantitative Data Collection
The CSFs for the adoption of the HMIS questionnaire comprised six sections. Section A comprised general demographic questions such as age, gender, department, qualifications, and experience with computer systems. These generally helped to show the coverage of the employees who participated in the study and helped to demonstrate the randomness of the process of respondent selection. Section B was designed to solicit information about technological factors, while Section C was designed to collect information on organizational factors and Section D to cover environmental factors. Section E was designed to cover individual factors and Section F was designed to cover general hospital operations. A 5-point Likert scale was used with 1 denoting strongly disagree and 5 denoting strongly agree to rate the questions in the main sections of the questionnaire.
The total number of distributed questionnaires was 360 as per the calculated sample size distributed to 3 participating institutions, and each had an allocation of 120 questionnaires. At the end of the data collection period, 122 questionnaires were deemed usable from those received. Usable questionnaires are those that were correctly filled in and with missing information, if any, deemed to be insignificant to distorting the results. The participant profile is given in Table 2.
Table 2
Participants profile for critical success factors questionnaire
| Variable | Classification of variables | Frequency | Percentage |
|---|---|---|---|
| Sex | Male | 39 | 32.0 |
| Female | 83 | 68.0 | |
| Age (yr) | 18-25 | 23 | 18.9 |
| 25-30 | 35 | 28.7 | |
| 30-39 | 21 | 17.2 | |
| 39-49 | 25 | 20.5 | |
| >49 | 18 | 14.8 | |
| Education | Doctorate | 3 | 2.5 |
| Masters | 4 | 3.3 | |
| Undergraduate | 33 | 27.0 | |
| Diploma | 68 | 55.7 | |
| Certificate | 12 | 9.8 | |
| Other | 2 | 1.6 | |
| Job title | Nurse | 69 | 56.6 |
| Physician | 13 | 10.7 | |
| Allied health | 7 | 5.7 | |
| Admin | 14 | 11.5 | |
| Technical services | 11 | 9.0 | |
| Specialist doctor | 8 | 6.6 | |
| Site | 1 | 47 | 38.5 |
| 2 | 39 | 32.0 | |
| 3 | 36 | 29.5 |
3.2.4.Quantitative Data Analysis
Inferential statistics techniques were used for the analysis of quantitative data. These techniques help researchers to draw conclusions and find trends in data about a population, helping them to study the connections between variables in a sample and to make generalisations and predictions about the relationships between the variables within the entire population. The inferential statistics used for this study included factor analysis, correlation analysis, and regression analysis.
3.3. Phase 2: Qualitative Data Collection and Analysis
This phase comprised sampling, data collection, and data analysis for the qualitative data collected, that is, for the CSF interviews.
3.3.1. Sampling
Purposive sampling was used for the CSF interviews. Those interviewed were senior personnel in the medical fraternity and a small number of participants from administration or service departments, namely, the medical superintendent, sisters-in-charge, accountants, human resource administrators, and IT personnel. The total number of participants interviewed was 10. This number was deemed sufficient and representative as there are generally fewer management and administrative staff members in relation to the entire staff complement at the hospital.
3.3.2. Qualitative Data Collection
Ten interviews were held with the senior staff and administrators in the selected institutions. Semi-structured in-depth interviews were used to collect data on the factors influencing the adoption of HMISs from a managerial viewpoint and on the role played by the technological, environmental, organizational, and individual factors. The interviews were held at times convenient to the participants and at their places of work so as not to inconvenience their work schedules and to minimise costs for the researcher. The researcher interviewed two participants from one hospital and four participants from each of the other two hospitals. All interviewees agreed to accommodate follow-up questions by e-mail or telephone if clarity on their responses was needed. The participants’ profile is shown in Table 3.
Table 3
Summary of participant profile
| Variable | Classification of variables |
Frequency |
|---|---|---|
| Sex | Male | 4 |
| Female | 6 | |
| Age (yr) | 18-25 | 0 |
| 25-30 | 1 | |
| 30-39 | 3 | |
| 39-49 | 4 | |
| >49 | 2 | |
| Education | Doctorate | 1 |
| Masters | 2 | |
| Undergraduate | 4 | |
| Diploma | 2 | |
| Certificate | 0 | |
| Other | ||
| Site | 1 | 4 |
| 2 | 4 | |
| 3 | 2 |
3.3.3. Qualitative Data Analysis
The thematic analysis technique was used to analyse the data collected during the in-depth interviews. Crowe et al. (2015) define thematic analysis as the procedure of analysing qualitative data to discover patterns of meaning. To analyse qualitative data using thematic analysis, themes are identified in the data, labelled, organised, and analysed, with the findings finally being reported on. The data analysis software R-QDA ( https://rqda.r-forge.r-project.org/) was employed in analysing the qualitative data.
The analysis procedure for the qualitative data was a combination of content and thematic analysis. The process went through the familiarisation, identification of a thematic framework, coding, charting, mapping, and interpretation stages, which were performed beyond describing what participants said. The ten interview scripts were converted into ten plain text documents and loaded into R-QDA software. Codes and code categories were created based on the information obtained from the review of literature and the underpinning theory. The codes were generated from the conceptual model and hypotheses and matched with emerging themes from the scripts, as shown in Table 4.
Table 4
Summary of themes, subthemes, and codes
| Code | No. ofinterviewees | No. ofmentions | Sub themes | Themes |
|---|---|---|---|---|
| External support | 10 | 22 | Government support NGOs and corporate support Financial support Human resource support |
Need for financial and resources support from government and corporates (Partners) |
| Technology support infrastructure | 10 | 21 | Need for adequate or requisite infrastructure Support for acquisition Support for installation Support for technology shareability Policy and regulation |
Supporting infrastructure development |
| government regulation and policy | 10 | 22 | Policy pushes for technology use Political environment necessary for technology boom Executive support Legislature support |
Government policies and regulation at the core of adoption |
| Industry and competitive pressure | 0 | 0 | Horizontal integration Vertical Integration Industry standardisation |
Integration of departments and with outside organizations |
| Market scope | 6 | 6 | Technology to suit clients’ needs How related organizations are dealing with same technology Reach of clients |
Market focus determines choice |
| Technology availability | 10 | 15 | Availability on market Affordability of technology Availability of funds |
Availability, affordability, and availability of capital |
| Technology relative advantage | 10 | 52 | Improved processes and user benefits Increased revenue/ Decreased costs Client satisfaction |
Technology brings more benefits than costs |
| Technology compatibility | 10 | 12 | Equipment compatibility Process compatibility Values compatibility Human resource compatibility |
How technology fits into organization |
| Technology trialability | 10 | 13 | Pre-testability Pre-implementation installation Possibility of scaled implementation |
Certification of product before implementation |
| Technology observability | 10 | 12 | Understanding the value of a technology through: Personal experience Third party experience |
Identification and visualization of benefits |
| Technology complexity | 10 | 12 | Scale of systems (components, people) System features complexity Processes complexity |
Inter-dependence of components, routines, individuals, and resources |
| Management support and practices | 10 | 17 | Management practices and priorities Resource mobilization & provision Participation |
Importance of management activities |
| Organizational size | 3 | 3 | Organizational size measured as: Departmental size Staff size |
Size’s effects on organizational activities |
| Organizational communication processes | 10 | 23 | Communication channels Adequate information & Relevant information |
Communication processes |
| Organizational readiness | 10 | 27 | Patient readiness Members’ readiness Resources availability |
Organizational components readiness |
| Organizational ICT expertise | 10 | 35 | In-house expertise Training possibility Hiring possibility |
Knowledge on organizational ICT systems |
| Perceived ease of use | 10 | 16 | Systems learnability Interface usability System trainability |
Effort at using the system |
| Perceived usefulness | 10 | 23 | Benefits or usefulness Extend of benefits derived versus cost Functionality User needs compared to system functions |
Technology solves the current problems |
| Subjective norm | 3 | 1 | The need to keep in line with trends can also affect decisions Individual norm Organizational norm |
Norms of other organizations |
| Attitude | 10 | 19 | Attitudes of members can affect adoption personal attitude Group attitude |
Feelings about the technology |
| Intention to use | 10 | 21 | Possibility of resistance to system Personal willingness Group willingness |
Willingness and readiness to use |
3.4. Phase 3: Model Confirmation
In this phase, another set of data was collected in order to confirm the results that had been collected in the first two phases and to clarify all discrepancies.
3.4.1. Sampling
Purposive sampling was the choice of the researchers in selecting respondents for the questionnaire designed to evaluate the HMIS adoption model, as the researcher sought participants who had managerial and ICT insights.
3.4.2. Data Collection
The evaluation questionnaire was made up of closed and open-ended questions. The questionnaire was made up of six sections, which were designed for evaluating the fit of the various factors in the model. The first section was designed to test for the general agreement of the participants with the model’s adequacy, completeness, and applicability. The second section was used to confirm the organizational factors, while the third section was used to confirm the technological factors. The fourth section was used to confirm the environmental factors, and the fifth to confirm the individual factors. The sixth section was used as an open-ended questionnaire for use in clarification of their choices by the participants. The outcome would confirm the results from the first two data sets. For the structured questions, the researcher chose to use a five-point Likert scale rating.
The participants included 36 hospital staff and four academic experts (employed in the academic field and with an interest in adoption studies as shown by their publications). The researcher contacted the participants and sought their consent. Those who indicated their willingness were sent the questionnaire together with the informed consent form by electronic means. Thirty-one (31) questionnaires were returned in total and were usable, of which 28 were from hospital employees while three were from academic experts.
3.4.3. Data Analysis
3.4.3.1. Correlation Analysis.
Correlation provides a picture of the association or lack of it between two variables of interest, which can be positive or negative. If the two variables’ relationship moves in one direction, that is, a decrease in one variable corresponds to a decrease in the other variable or vice-versa, then the relationship is deemed to be positive; if the variables move in opposite directions, that is, an increase in one variable corresponds to a decrease in another or vice-versa, then the relationship is deemed to be negative. There are various correlation tests that can be used in data analysis, and these include the Spearman’s rank, Karl Pearson’s product-moment, the coefficients of concurrent deviations, or scatter diagrams (Sereno, 2021). Correlation tests were performed on the confirmation questionnaire as a way of proving the relationships that had been identified through the CSF questionnaire and the interviews.
3.5. Reliability and Validity
Reliability and validity were ensured by monitoring the parameters of the instruments to maintain the same properties. A pilot test was used to ensure reliability by giving the instrument to different respondents in different health institutions to check the consistency of the results prior to the main data collection exercise. Validity can be ensured in two ways, namely internal and external. Internal validity ensures the obtained results are legitimate, and for this study it was ensured by the way that the respondents were selected (health workers), and the way that the data was handled, i.e., recorded and analysed.
The sampling criteria used provided the ability to externally validate or generalise the results. Although random sampling was used, the information can be deemed to be reliable to localisation of the research to a particular area where the respondents were typical or representative of the whole population. A high level of validity (internal and external) was achieved through strict protocol execution and study design.
4. RESULTS
The results of the analysis are presented in this section.
4.1. CSF Questionnaire Results
The 122 completed questionnaires were captured into IBM SPSS statistics 20 for analysis and the results are presented below:
4.1.1. CSF Questionnaire Instrument Validation
Construct validity was performed using factor analysis. The techniques applied include principal-components factor analysis, extraction technique, and varimax orthogonal rotation method. To achieve a reliable scale from the available set of survey items, the Cronbach’s alpha coefficient of internal consistency had to be determined. Reliability can be guaranteed for higher values of the Cronbach’s alpha, which has a range of 0-1. The factor loadings for the factors accepted for further tests range from 0.640 to 0.955, which meet the recommended minimum value of 0.5 suggested by Chin et al. (1997) (Table 5).
Table 5
Factor analysis results
| Construct | Sub-construct | Items included | Cronbach’s alpha |
|---|---|---|---|
| Environmental | External support | ESP 2-5 | 0.804 |
| Government regulation and policy | GR 3-4 | 0.854 | |
| Industry and competitive pressure | PRES 2-3 | 0.922 | |
| Technological | Availability | TA 5-7 | 0.766 |
| Relative advantage | RA 1-3 (organization) | 0.895 | |
| RA 5-11 (patients) | 0.854 | ||
| Compatibility | CBT 1-2 | 0.655 | |
| Observability | OB 1-2 | 0.737 | |
| Organizational | Support and skills | 0.929 | |
| Organizational readiness (general) | OR 5-6 & SI 1-2 | 0.807 | |
| Organizational readiness (aim/vision) | OR 2, 4 | 0.663 | |
| Individual | Usefulness and ease of use | PU 1-3 & PEOU 1-3 | 0.955 |
| Subjective norm | SN 1-2 | 0.685 | |
| Adoption | Adoption | F 2.3 & F 2.4 | 0.640 |
ESP, external support; GR, government regulation, PRES, industry and competitive pressure; TA, availability; RA, relative advantage 9; CBT, compatibility; OB, observability; OR, organisational readiness; SI, support and skills; PU, perceived usefulness; PEOU, perceived ease of use; SN, subjective norm; F, adoption.
The constructs retained after the Cronbach’s test were the ones deemed to be internally consistent. They were subjected to correlational and regression testing in a bid to come up with the existing relationships between the constructs and the DV as well as to ascertain the predictors of HMIS adoption. Those with a Cronbach’s value of less than 0.5 were not deemed to be internally consistent and hence were removed from further statistical testing, leaving only the remaining 13 constructs for further statistical analysis.
4.1.2. Hypotheses Test
Regression analysis was used to test the structural links of the research model and the results are presented in Table 6. The estimated coefficients are given along with the associated p-value. Calvello (2020) explains the use of correlation and regression as providing a quick and simple summary of the direction and strength of the relationship between two or more numeric values, looking to predict, optimise, or explain a number response between the variables, respectively.
Table 6
Hypotheses results
| Dependent variable |
Independent variable | Coefficient | Model | |||||
|---|---|---|---|---|---|---|---|---|
| Beta | p-value | R2 | F | df | p-value | |||
| Adoption | External support | -0.052 | 0.570 | 0.003 | 0.324 | 1; 120 | 0.570 | |
| Adoption | Government regulation and policy | -0.060 | 0.510 | 0.004 | 0.437 | 1; 120 | 0.510 | |
| Adoption | Industry and competitive pressure | -0.223 | 0.014* | 0.050 | 6.282 | 1; 120 | 0.014* | |
| Adoption | Availability | -0.047 | 0.606 | 0.002 | 0.268 | 1; 120 | 0.606 | |
| Adoption | Relative advantage-organization | -0.196 | 0.031* | 0.038 | 4.779 | 1; 120 | 0.031* | |
| Adoption | Relative advantage-patients | 0.044 | 0.631 | 0.002 | 0.232 | 1; 120 | 0.631 | |
| Adoption | Compatibility | -0.078 | 0.392 | 0.006 | 0.738 | 1; 120 | 0.392 | |
| Adoption | Observability | 0.052 | 0.571 | 0.003 | 0.324 | 1; 120 | 0.571 | |
| Adoption | Management support and skills | -0.263 | 0.003* | 0.069 | 8.952 | 1; 120 | 0.003* | |
| Adoption | Organizational readiness (general) | 0.036 | 0.692 | 0.001 | 0.158 | 1; 120 | 0.692 | |
| Adoption | Organizational readiness (aim/vision) | -0.111 | 0.224 | 0.012 | 1.497 | 1; 120 | 0.224 | |
| Adoption | Usefulness and ease of use | -0.003 | 0.978 | <0.0005 | 0.001 | 1; 120 | 0.978 | |
| Adoption | Subjective norm | -0.010 | 0.916 | <0.0005 | 0.011 | 1; 120 | 0.916 | |
The regression tests show the relationships between DVs and IVs. The closer the p-value is to 0, the stronger is the relationship, meaning that it affects adoption. The constructs were taken as the IVs with adoption as the DV. As indicated in Table 6, the tests showed the following ‘significant influences’ from the tested hypotheses:
-
The more agreement there is that industry and competitive pressure (external pressure) is good for the organization, the higher the adoption of HMIS technologies, p=0.014.
-
The more agreement that current technology gives the organization relative advantage, the higher the adoption of HMIS technologies, p=0.031.
-
The more agreement that there is management support and available skills, the higher the adoption of HMIS technologies, p=0.003.
4.1.3. Explaining the CSF Questionnaire Results
From the quantitative results, only three factors within the technological, organizational, and environmental context proved to be significant and to have an influence in the adoption of HMIS by public hospitals in Zimbabwe.
First, industry and competitive pressure (p=0.014) produced a significant result, showing that it influences the decision to adopt. This has been demonstrated in various studies, such as that by Zhang et al. (2013), who studied the elements responsible for the adoption of Health Information Technology in US acute care hospitals and found competitive pressure given as market competition as one of the factors. Secondly, management support (p=0.03) was shown to be a critical factor for adoption of HMISs and this is consistent with the studies of Oliveira et al. (2014) and Borgman et al. (2013) in cloud adoption studies. Oliveira stated that by providing financial and other resources, top management would show support for the adoption of cloud computing. The third significant factor for the adoption of HMISs was relative advantage (p=0.031), and this is in line with studies by Premkumar and Roberts (1999) in the adoption of innovative information technologies by enterprises, by Sin Tan et al. (2009) in the adoption of online data access, and by Zhu et al. (2006) in the study of digital transformation for European companies.
These three significant factors have been proven in previous studies while the other hypotheses failed to hold. However, this is in line with the previous conclusions of other researchers, who stated that each study setting can have its own set of constructs that are unique to the technology and organization under study. This view is upheld by Oliveira and Martins (2011, p. 112) who stated: “The TOE framework has a solid theoretical basis, consistent empirical support and the potential of application to IS innovation domains, though specific factors identified within the three contexts may vary across different studies.” An example of variations within the three contexts of the TOE model was reported by Ruivo et al. (2016), who proposed a model with five constructs: compatibility and training as technological factors; size and best practices as organizational factors; and competitive pressure as an environmental factor. Another example was reported by Chiu et al. (2017) in their study of adoption of broadband by enterprises, which revealed that the significant factors were as follows: relative advantage, trialability, observability, and compatibility within the technological context; information intensity, top management support, employees’ knowledge, and absorptive capability within the organizational context; and business partners, competitive pressure, and external support within the environmental context.
4.2. CSF Interview Results
This section presents the results of the interviews for answering the research questions and hypotheses.
After the coding of the responses from the interviewees, the themes and codes were identified and used to answer the research questions, as shown in Table 7. All the identified themes were mapped to one or more identified codes.
Table 7
Themes, codes, and RQ
| RQ | Supporting themes | Matching codes |
|---|---|---|
| RQ1: What are the environmental factors that influence the adoption of HMIS in Zimbabwean healthcare institutions? | Theme 1: Need for financial and resource support from government and corporates (partners) | External support |
| Theme 2: Supporting infrastructure development | Support infrastructure | |
| Theme 3: Government policies and regulation at the core of adoption | Government support | |
| Theme 4: Integration of departments and partnerships with outside organizations | Market scope | |
| Theme 5: Market focus determines choice | Industry and competitive pressure | |
| RQ2: What are the technological factors that influence the adoption of HMIS in Zimbabwean healthcare institutions? | Theme 6: Availability, affordability, and availability of capital | Relative advantage |
| Theme 7: Technology brings more benefits than costs | Trialability | |
| Theme 8: How technology fits into the organization | Technology availability | |
| Theme 9: Certification of product before implementation | Observability | |
| Theme 10: Identification and visualisation of benefits | Compatibility | |
| Theme 11: Inter-dependence of components, routines, individuals, and resources | Complexity | |
| RQ3: What are the organizational factors that influence the adoption of HMIS in Zimbabwean healthcare institutions? | Theme 12: Importance of management activities | Management support |
| Theme 13: Size’s effects on organizational activities | Size | |
| Theme 14: Communication processes | Communication processes | |
| Theme 15: Organizational components readiness | Organizational readiness | |
| Theme 16: Knowledge on organizational ICT systems | ICT expertise | |
| RQ4: What are the individual factors influencing the adoption of HMIS in Zimbabwean healthcare institutions? | Theme 17: Effort in using the system | PEOU |
| Theme 18: Technology to solve the current problems | PU | |
| Theme 19: Feelings about the technology | Attitude | |
| Theme 20: Willingness and readiness to use | Intention to use |
The results showed that environmental (external support, support infrastructure, government support, market scope, industry and competitive pressure), technological (relative advantage, trialability, technology availability, observability, compatibility, complexity), organizational (management support, size, communication processes, organizational readiness, ICT expertise) and individual factors (PEOU, PU, attitude, intention to use) do have an influence on the adoption of HMIS in Zimbabwe, as shown in Table 7.
More information on themes, sub-themes, and codes is provided in Table 4. All the codes and themes answer all four research questions as well as the fifth research question (“How can the CSFs be integrated into an adoption model for HMIS in public health institutions in Zimbabwe?”), helping us to come up with a model that explains the factors at play in the organization’s adoption of technology, as shown in the Fig. 4.
Fig. 4
Final health management information system adoption model. ICT, information and communication technology.
4.3 Model Confirmation Results
Because of the discrepancy between the CSF questionnaire and CSF interview results and in order to achieve completeness, complementarity, and triangulation, another instrument was designed and administered. The results of the two methods of correlation and thematic analyses are presented in the two sections below.
4.3.1. Confirmation Correlation Analysis
The quantitative part of the questionnaire was analysed using the Wilcoxon signed ranks test (non-parametric equivalent to the one-sample t-test), in which the median is tested against the central score of ‘3’ to determine significance of agreement or disagreement.
The tests conducted proved that there is significant agreement that organizational factors are important for adoption of HMISs (communication processes M=4.52, p<0.0005; management support M=4.35, p<0.005 & M=4.29, p<0.005; organizational readiness M=4.48, p<0.005 & M=4.39; and ICT expertise M=4.65, p<0.005).
The results also show that there is significant agreement that technological factors are important for adoption, as shown by the mean scores and the Wilcoxon signed ranks test (relative advantage M=4.55, p<0.005; trialability M=4.29, p<0.005; observability M=4.16, p<0.005 & M=3.84, p<0.005; availability M=3.77, p<005 & M=4.06, p<005; compatibility M=4.29, p<0.005 & M=4.26, p<005; and technology complexity M=4.13, p<0.005 & M=3.94, p<0.005).
The environmental factors important for adoption of an HMIS are as follows: external support policies M=4.13, p<0.005; government regulation M=4.16, p<0.005 & M=4.13, p<0.005; industry and competitive pressure M=3.81, p<0.005 & M=4.35, p<0.005 & M=4.06, p<0.005; and technology infrastructure support M=4.26, p<0.005 & M=4.35, p<0.005 & M=4.19, p<0.005.
The individual factors important for adoption of an HMIS are as follows: PU M=4.35, p<0.005; PEOU M=3.81, p<0.005; attitude M=4.13, p<0.005; and intention to use M=4.19, p<0.005. Thus, they are important and are integrated in the final model based on these results.
4.3.2. Confirmation of Main Factors Significance
Reliable composite measures were computed for the main factor levels, namely organization, technology, environment, and individual, to measure the significance of the main factors for adoption of HMIS. The results are given in Table 8.
Table 8
Main factor level test results
| Factor | Items included | Cronbach’s alpha | Mean agreement score | p-value (testing for sig agreement/disagreement) |
|---|---|---|---|---|
| Organizational | 2.1-2.6 | 0.929 | 4.45 | <0.0005 |
| Technological | 3.1-3.3, 3.5-3.7, 3.9-3.10 | 0.753 | 4.09 | <0.0005 |
| Environmental | 4.1-4.3, 4.5-4.9 | 0.844 | 4.21 | <0.0005 |
| Individual | 5.1-5.4 | 0.843 | 4.12 | <0.0005 |
The results show that the participants agreed that the organizational (M=4.45, p<0.005), environmental (M=4.21, p<0.005), technological (M=4.09, p<0.005), and individual (M=4.12, p<0.005) factors are important for adoption of HMIS.
The confirmation results support the results from the quantitative and qualitative results, giving the model output shown in Fig. 4.
4.4. Summary of the Results
The results of the CSF questionnaire proved only three factors as significant for the adoption of HMIS, namely, the environmental factor construct of industry and competitive pressure, the technological factor construct of relative advantage, and the organizational factor construct of management support and available skills. The interview data showed that the following factors influenced HMIS adoption in public hospitals in Zimbabwe: the organizational factor constructs of communication processes, management support, organizational readiness, and ICT expertise; the technological factor constructs of technology availability, relative advantage, compatibility, complexity, trialability, and observability; the environmental factor constructs of external support, technology infrastructure support and government regulation; and the individual factor constructs PEOU, PU, attitude, and intention. Because of the discrepancy between the results of the interviews and the questionnaires, a third instrument was designed, including constructs that had been validated in either the interviews or the questionnaire. The set of the constructs were validated as shown in the HMIS model in Fig. 4.
5. DISCUSSION AND RECOMMENDATIONS
Several conclusions can be drawn from the results presented, and these pertain to the research objectives. Although the sample from which data was gathered is small, especially for qualitative data, the researcher believes that the results provide meaningful insights that could be generalised to adoption experiences of HMIS in public health institutions in Zimbabwe.
The idea of adoption, while seemingly straightforward, is a complex process with many factors at play, as has been shown by the unification of different models or theories to try to explain the phenomena. The results of this study have demonstrated that organizational adoption of HMISs can be influenced by technological, organizational, environmental, and individual factors. The technological, organizational, and environmental factors have been proved by the research done by Tornatzky and Fleischer (1990), and it has been shown that the actual antecedents of these broad factors vary from one setting to another as shown by the removal of the sub-constructs of the market scope under (H1) and size under H3. This may be due to the nature of the industry, where they are driven by government policies rather than industry standards and client demands. This has also been proved by many studies that have used the TOE model, which come up with different antecedents for the three factors. There is a direct path for technological adoption (H2), organizational factors (H3), and environmental factors (H1). This agrees with studies conducted by Kuan and Chau (2001), Ramdani and Kawalek (2007), Zhu and Kraemer (2005), Zhu et al. (2002), and Zhu et al. (2006), all using the TOE model for the adoption of various technologies, although with varying sub-constructs depending on the technology and other business settings.
Baker (2012) suggests that there is a need to explore ways to evolve the TOE model and find out how individual behaviors and adoption can affect organizational adoption. Accordingly, the researcher included individual factors and they have been proved to have an indirect effect on technological decision making through attitude (H4), which has a direct effect on intention to use (H7), which directly influences decisions on technology adoption. The individual factors from TRA and TRB were shown to affect the adoption of innovation at the organizational level. This is shown by the acceptance of the PEOU and PU in the research results. This shows that there is an interplay of more factors that affect how organizations adopt technology than those stated in the TOE model. Thus, although the TOE model can be useful in interpreting how organizations adopt IT innovations, it does not fully show how the individual behaviors of members can contribute to the adoption matrix. There have been many studies that try to complement the TOE model, but none have used individual/behavioral factors as in this research study.
Most adoption/acceptance studies have separated individual/behavioral studies from organizational studies, with the assumption that adoption in an organization is either on an organizational level or an individual level. At the organizational level, the studies have assumed that when an organization adopts an innovation, the employees have no choice but to use what the organization has adopted; with behaviorbehavioral studies, the assumption is that the use of the technology is not mandatory, and users have the choice to use or reject. In the studies carried out previously, the two adoption phases are recognized as two distinct processes, which do not interact. However, it appears that the two are related and should be treated as a continuum and that, when studies are carried out, they should be undertaken at the same time, especially for mandatory environments. The success of an adoption of an innovation should be measured by implementation and continued use. In this way, the behavioral aspects of the use of the technology would be known and could reduce the chances of the use of the technology being discontinued after adoption (Weng et al., 2018).
Researchers should study the adoption of organizational innovations with individual acceptance in mind, as individual employees can cause disruptive tendencies after organizations adopt a technological innovation. Managers of adoption should also assess all possible factors that can affect the success of the adoption process and should not concentrate on technological, organizational, and environmental factors only but should, in addition, assess the behaviorbehavioral factors of the individuals within the organization. The traditional approach of separating organizational from individual adoption and treating them as primary and secondary should be discontinued to allow the success rate of technological adoption to increase and, more importantly, to enable the impact of adopted technologies for the health sector to result in improved organizational processes and ultimately high-quality patient care.
Hospitals are recommended to implement the HMIS technology as it allows for improved service delivery. The use of HMIS will allow for streamlined resource allocation, effective management and monitoring, and consequently its use will allow for improved services to the patients. Resources are a challenge and hospitals can come up with fundraising initiatives such as billing the patients towards the implementation of the HMIS, so as to improve service delivery through technology. There is a need to integrate the use of ICTs in the curriculum of health professionals’ training so as to improve their chances of accepting technology when it is integrated into their environments.
REFERENCES
, , , (2016) Critical factors influencing decision to adopt human resource information system (HRIS) in Hospitals PLoS One, 11(8), e0160366 https://doi.org/10.1371/journal.pone.0160366. Article Id (pmcid)
, , (2015) Knowledge and utilization of computers among health professionals in a developing country: A cross-sectional study JMIR Human Factors, 2(1), e4 https://doi.org/10.2196/humanfactors.4184. Article Id (pmcid)
(2017) Determinants of routine health information utilization at primary healthcare facilities in Western Amhara, Ethiopia Cogent Medicine, 4, 1387971 https://doi.org/10.1080/2331205X.2017.1387971.
(2020) Correlation vs. regression made easy: Which to use + why https://online210.psych.wisc.edu/wp-content/uploads/PSY-210_Unit_Materials/PSY-210_Unit12_Materials/Calvello_Regression_2020.pdf
, , (1997) Advancing the theory of adaptive structuration: The development of a scale to measure faithfulness of appropriation Information Systems Research, 8(4), 342-367 http://www.jstor.org/stable/23010917.
, , (2017) International Journal of Management, Economics and Social Sciences (Vol. 6) An integrated perspective of TOE framework and innovation diffusion in broadband mobile applications adoption by enterprises, 1, pp. 14-39, http://hdl.handle.net/10419/157921
, , (2015) Conducting qualitative research in mental health: Thematic and content analyses Australian and New Zealand Journal of Psychiatry, 49(7), 616-623 https://doi.org/10.1177/0004867415582053.
(1989) Perceived usefulness, perceived ease of use, and user acceptance of information technology MIS Quarterly, 13(3), 319-340 https://doi.org/10.2307/249008.
, , , , , , , , (2020) Perceptions of factors influencing the introduction and adoption of electronic immunization registries in Tanzania and Zambia: A mixed methods study Implementation Science Communications, 1, 38 https://doi.org/10.1186/s43058-020-00022-8. Article Id (pmcid)
, , (2001) Physicians' adoption of information technology: A consumer behavior approach Health Marketing Quarterly, 19(2), 3-21 https://doi.org/10.1300/J026v19n02_02.
(2018) The challenges of technology adoption in healthcare https://pharmaboardroom.com/articles/the-challenges-of-technology-adoption-in-healthcare/
, (2018) Factors influencing e-health implementation by medical doctors in public hospitals in Zimbabwe South African Journal of Information Management, 20(1), a928 https://doi.org/10.4102/sajim.v20i1.928.
, , , (2010) Critical factors of hospital adoption on CRM system: Organizational and information system perspectives Decision Support Systems, 48(4), 592-603 https://doi.org/10.1016/j.dss.2009.11.009.
(2018) Empirical study of Nova Scotia nurses' adoption of healthcare information systems: Implications for management and policy-making International Journal of Health Policy and Management, 7(4), 317-327 https://doi.org/10.15171/ijhpm.2017.96. Article Id (pmcid)
International Center for AIDS Care and Treatment Programs at Columbia University (2015) In Lesotho, new health information system provides streamlined, integrated data across health programs https://icap.columbia.edu/news-events/in-lesotho-new-health-information-system-provides-streamlined-integrated-data-across-health-programs/
, (2011) Comparison of contemporary technology acceptance models and evaluation of the best fit for health industry organizations International Journal of Computer Science Engineering and Technology, 1(11), 709-717 https://ijcset.net/docs/Volumes/volume1issue11/ijcset2011011106.pdf.
, , (2020) Factors influencing district health information system usage in Sierra Leone: A study using the technology-organization-environment framework Electronic Journal of Information Systems in Developing Countries, 86(6), e12140 https://doi.org/10.1002/isd2.12140.
, , , , , (2008) Factors influencing physician use of clinical electronic information technologies after adoption by their medical group practices Health Care Management Review, 33(4), 361-367 https://doi.org/10.1097/01.HCM.0000318773.67395.ce.
, (2001) A perception-based model for EDI adoption in small businesses using a technology-organization-environment framework Information & Management, 38(8), 507-521 https://doi.org/10.1016/S0378-7206(01)00073-8.
, (2013) Antecedents of open source software adoption in health care organizations: A qualitative survey of experts in Canada International Journal of Medical Informatics, 82(8), 731-741 https://doi.org/10.1016/j.ijmedinf.2013.04.001.
, (2011) Literature review of information technology adoption models at firm level Electronic Journal of Information Systems Evaluation, 14(1), 110-121 https://academic-publishing.org/index.php/ejise/article/view/389.
, , (2014) Assessing the determinants of cloud computing adoption: An analysis of the manufacturing and services sectors Information & Management, 51(5), 497-510 https://doi.org/10.1016/j.im.2014.03.006.
, (2014) Factors affecting electronic medical record system adoption in small Korean hospitals Healthcare Informatics Research, 20(3), 183-190 https://doi.org/10.4258/hir.2014.20.3.183. Article Id (pmcid)
, (1999) Adoption of new information technologies in rural small businesses Omega, 27(4), 467-484 https://doi.org/10.1016/S0305-0483(98)00071-1.
, (2016) Role of hospital information systems in improving healthcare quality in hospitals Indian Journal of Science and Technology, 9(26), 1-5 https://doi.org/10.17485/ijst/2016/v9i26/92686.
, , , (2016) Factors that influence the implementation of e-health: A systematic review of systematic reviews (an update) Implementation Science, 11(1), 146 https://doi.org/10.1186/s13012-016-0510-7. Article Id (pmcid)
RTI International (2014) Zimbabwe launches new health information system (HIS) http://static.ictedge.org/node/975.html
RTI International (2021) Improving health service delivery through a national health information system and mobile-based disease reporting https://www.rti.org/impact/zimbabwe-health-information-and-support-project-zimhisp
, , , , (2016) Using TOE and RBV theories to define a theoretical model to assess ERP value across Iberian manufacturing and services SMEs Procedia Computer Science, 100, 474-479 https://doi.org/10.1016/j.procs.2016.09.184.
Sereno (2021) Comparison of Pearson and Spearman correlation coefficients https://www.analyticsvidhya.com/blog/2021/03/comparison-of-pearson-and-spearman-correlation-coefficients/
(2013) User centric cloud service model in public sectors: Policy implications of cloud services Government Information Quarterly, 30(2), 194-203 https://doi.org/10.1016/j.giq.2012.06.012.
, , , (2009) Internet‐based ICT adoption: Evidence from Malaysian SMEs Industrial Management & Data Systems, 109(2), 224-244 https://doi.org/10.1108/02635570910930118.
Techzim (2014) Zim hospitals introduce a new e-health system: How does it work? https://www.techzim.co.zw/2014/10/zim-hospitals-introduce-new-e-health-system-work
United Nations Development Programme (UNDP) (2014b) Electronic patient management system ePMS - Zimbabwe https://www.undp.org/sites/g/files/zskgke326/files/migration/zw/UNDP_ZW_HIVAIDS_epms_zimbabwe.pdf
United Nations Development Programme (UNDP) (2020) Healthy systems for healthy people: UNDP and Global Fund support to strengthen the national health management information system https://www.undp.org/sites/g/files/zskgke326/files/migration/zw/UNDP_ZW_GF_HMIS.pdf
, (2000) A theoretical extension of the technology acceptance model: Four longitudinal field studies Management Science, 46(2), 186-204 https://doi.org/10.1287/mnsc.46.2.186.11926.
, , , , (2005) Factors influencing health information system adoption in American hospitals Health Care Management Review, 30(1), 44-51 https://doi.org/10.1097/00004010-200501000-00007.
, , (2012) ICT attributes as determinants of e-commerce adoption by formal small enterprises in urban Kenya International Journal of Business and Social Science, 3(23), 65-74 https://www.researchgate.net/publication/262794622_ICT_Attributes_as_Determinants_of_E-commerce_Adoption_by_Formal_Small_Enterprises_in_Urban_Kenya.
, , , (2018) A TAM-based study of the attitude towards use intention of multimedia among school teachers Applied System Innovation, 1(3), 36 https://doi.org/10.3390/asi1030036.
, , , , , (2013) Health information technology adoption in U.S. acute care hospitals Journal of Medical Systems, 37(2), 9907 https://doi.org/10.1007/s10916-012-9907-2.
, , , , , (2019) Assessment of the social influence and facilitating conditions that support nurses' adoption of hospital electronic information management systems (HEIMS) in Ghana using the unified theory of acceptance and use of technology (UTAUT) model BMC Medical Informatics and Decision Making, 19(1), 230 https://doi.org/10.1186/s12911-019-0956-z. Article Id (pmcid)
, (2005) Post-adoption variations in usage and value of e-business by organizations: Cross-country evidence from the retail industry Information Systems Research, 16(1), 61-84 http://www.jstor.org/stable/23015765.
, , , (2006) Innovation diffusion in global contexts: Determinants of post-adoption digital transformation of European companies European Journal of Information Systems, 15(6), 601-616 https://doi.org/10.1057/palgrave.ejis.3000650.
- Submission Date
- 2022-05-24
- Revised Date
- 2023-03-14
- Accepted Date
- 2023-03-15

